Surgical Technique Applying Mosquito Forceps to Galeotomies for Scalp Reconstruction
Article information
Abstract
Reconstruction of scalp defects can be difficult due to the stiffness and inelasticity of the scalp, posing challenges for surgeons. Galeotomies can be applied to allow for this inelastic tissue to stretch, increasing local tissue movement and reducing tension on wound margins, but they generally require large incisions and dissections. Here, we completely repaired scalp defects by applying a surgical technique for galeotomies that only required small incisions of the scalp using simple mosquito forceps. This study included nine patients who underwent scalp reconstruction for defects due to mass excision; all surgeries were performed by the same surgeon. All surgical wounds completely recovered with a satisfactory aesthetic outcome, with no notable complications during a mean follow-up period of 21 months. Taken together, our results showed that galeotomies can be successfully performed even in a confined space using mosquito forceps, offering an effective modality for reconstruction of medium-sized scalp defects with minimal complexity.
Introduction
Successful scalp reconstruction depends on a deep understanding of how the unique anatomy of the scalp affects tissue movement. The scalp is an important structure that contains the thickest integument in the human body, with its thickness ranging from 8 to 13 mm. There are five layers to the scalp: the skin, a connective tissue layer, the galea aponeurosis, a loose areolar tissue layer, and the pericranium. The galea aponeurosis in particular is an inelastic structure that restricts the movement of the upper skin and tightens the scalp [1,2]. Additionally, it contributes to the thickness and inelasticity of the scalp, thereby impeding stretching and lifting movements, making it difficult to transpose or advance tissue during surgery [3,4].
Since the scalp lacks tissue distensibility, a significant amount of tension can build up during scalp wound closure. This excessive tension during wound closure can lead to various complications, including wound dehiscence and alopecia due to loss of hair follicles [1-4]. Thus, tension-free closure is essential for successful and stable scalp reconstruction.
Many methods have been proposed for reducing tension during scalp wound closure. Multiple parallel linear incisions of the galea aponeurosis, also referred to as galeotomies or galeal scoring, are one of the methods used to stretch this inelastic tendon sheet, increase local tissue movement, and reduce tension [5,6]. However, caution is needed when performing a galeotomy, as well as a clear view of the galea undersurface, as there is a risk of both bleeding and vascular compromise if the incision cuts too deep into the vessels of the subcutaneous tissue [5]. Therefore, in many cases of scalp reconstructions using a galeotomy, the flap requires a large incision, and must be turned over to provide a clear view of the undersurface of the galea in order to avoid the risk of vascular damage [6]. However, it is not easy to ensure enough space for direct undersurface visualization in galeotomies that require only small incisions, such as in primary closure and advancement flaps. In addition, complicated flap designs and large incisions increase the operation time, difficulty of surgery, and risk of complications, including bleeding and alopecia.
Here, we devised a surgical technique for successful galeotomy requiring only a small incision of the scalp using simple mosquito forceps. We describe our successful technique and discuss the use of galeotomies for the reconstruction of moderate scalp defects.
Idea
Patients
The study population included nine patients who had scalp defects due to mass excision reconstructed by a single surgeon at our plastic surgery clinic from March 2020 to December 2022. The medical records of the patients were retrospectively reviewed to obtain pre- and postoperative demographic and clinical data. Updated information on postoperative complications was obtained from all patients via telephone or outpatient visits. This study was approved by the Institutional Review Board of Daegu Fatima Hospital (IRB No. 2023-03-001) and performed in accordance with the principles of the Declaration of Helsinki. All participants provided written informed consent.
The age of the patients ranged between 30 and 81 years. Two patients were males, and seven were females. Based on biopsies performed on the excised mass, malignant and benign tumors were identified in three and six patients, respectively. The locations of the scalp defects were classified into the frontoparietal/vertex, temporal/temporoparietal, and occipital areas. General anesthesia was used in two cases, whereas local anesthesia was used in seven cases. All patients were prescribed oral antibiotics for 5 days after surgery (Table 1).
Surgical technique
The entire scalp of the patient was disinfected with 10% povidone iodine. The boundary of the mass was marked using gentian violet and an elliptical excision line was designed. After making a skin incision along the planned incision line and removing the mass from the surrounding tissues using Metzenbaum scissors, the adhered galea aponeurosis was collectively excised. Through the defect margin, the avascular subgaleal plane was dissected using Metzenbaum scissors, and the undersurface of the galea was visualized by flap elevation. Firmly holding a no. 15 scalpel blade (Fig. 1A) using mosquito forceps so that its cutting edge faced the superior direction, the first coronal galeotomy was performed on the galea of the elevated flap approximately 1 cm from the wound margin. The flap was lightly pressed by hand to compensate for the insufficient tension between the galea and the blade, and the galea was incised while feeling the depth of the incision. At the same time care was taken not to cut the blood vessels above the galea (Fig. 1).

Surgical technique. (A) Mosquito forceps are used to fix the cutting edge of the no. 15 scalpel blade to face the superior direction. (B) After flap elevation, one hand is used to lightly press the flap to provide tension between the galea and the blade. Subsequently, galeotomy is performed while feeling the depth of the incision. In this way galeotomy can be performed effectively even in a narrow space since the blade edge can enter contact with the subgaleal area at an angle of approximately 90°. (C) Schematic diagram of the surgical technique.
After the first galeotomy, the next incisions were made as needed at 1-cm intervals further away from the wound margin. Galeotomies were performed in the same way on the flap on the opposite side of the defect, and approximation of the two flaps without tension was confirmed. After repairing the galea aponeurosis and subcutaneous tissue, the skin was closed with a simple interrupted suture, while care was taken to not generate excessive tension on the skin. The operation was finished after dressing the surgical site lightly with antibiotic ointment and foam.
Results
After mass excision, the skin defects varied in length, width, and area from 3.0 to 6.0 cm (mean, 4.27 cm), 2.2 to 4 cm (mean, 2.9 cm), and 7 to 24 cm2 (mean, 12.6 cm2), respectively. The galeal layer was exposed in all patients, but not the cranial bone. The operating time, including mass excision, ranged between 24 and 62 minutes (mean, 38.8 minutes). In six patients, the scalp defect was repaired in the first operation by galeotomies and primary closure. Meanwhile, one patient underwent revision surgery due to wound dehiscence. The other two patients needed additional wide excision due to malignant tumor identification by biopsy. These two patients underwent revisional surgery to repair the enlarged scalp defect by galeotomies and primary closure. Satisfactory outcomes were obtained in all patients during the 10- to 32-month follow-up period (mean, 21 months), without postoperative complications such as wound infection, wound dehiscence, recurrence, or hair loss (Table 2).
Illustrative case
A 53-year-old man was admitted to our plastic surgery department with a chief complaint of scalp mass. Preoperative punch biopsy of the mass identified it as a nevus sebaceus. Physical examination found a 4.5×2.8 cm well-defined, multilobulate, elevated mass in the left frontoparietal region (Fig. 2). We planned a mass excision under general anesthesia.
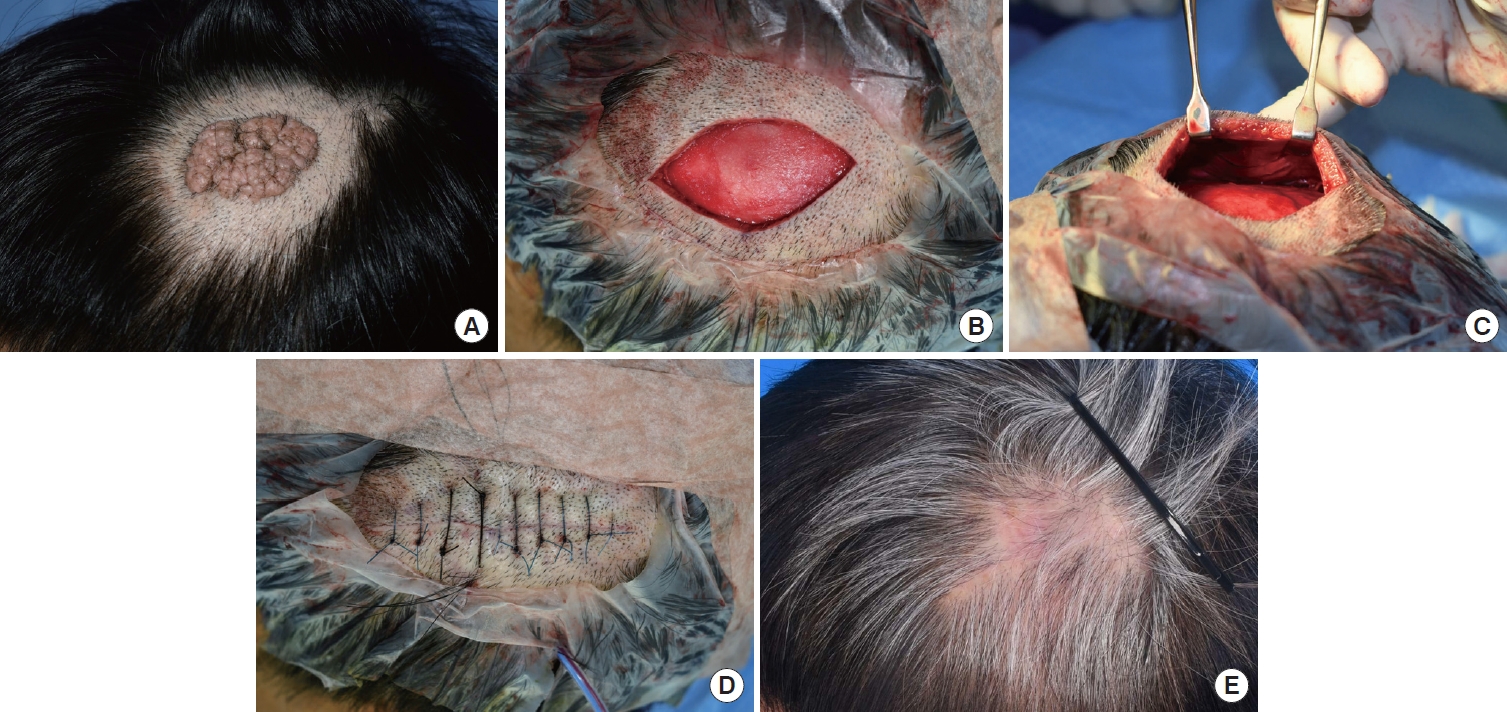
Illustrative case. (A) A 4.5×2.8 cm well-defined, multilobulate, and elevated mass observed in the left temporoparietal region was found during physical examination. (B) After total excision of the mass, the size of the skin defect was 6.0×4.0 cm, and the galeal layer was exposed. (C) Intraoperative photograph of three galeotomies parallel to the defect margin at an interval of 1 cm after elevation of the flap at the subgaleal plane. The galeotomies were used to facilitate additional scalp advancement. (D) Immediate postoperative photograph. After repairing the galea aponeurosis and subcutaneous tissue layer by layer, a drain was inserted. The scalp defect was closed without tension. (E) Photograph at 4 months postoperatively. During the 32-month follow-up, the patient recovered without wound infection, wound dehiscence, or recurrence.
Resection left a skin defect 6.0×4.0 cm in size. The avascular subgaleal plane under the superior edge of the defect was dissected using Metzenbaum scissors, and the undersurface of the galea was visualized by flap elevation. After fixing a no. 15 scalpel blade with mosquito forceps, three galeotomies were performed at 1-cm intervals starting from the wound edge, until the overlying subcutaneous fat was visible. Subsequently, three more galeotomies were performed on the lower side of the inferior edge of the defect using the same method, and the flap was approximated without tension.
The patient was discharged 2 days after surgery without complications, and total stitch removal was performed at postoperative 2 weeks in the outpatient plastic surgery clinic. The excised mass was again pathologically diagnosed as a nevus sebaceus. During the 31 months of follow-up, the patient was satisfied with the treatment results without any notable problems.
Discussion
Scalp reconstruction is challenging as it must satisfy both restoration of function and aesthetics. However, limited soft tissue expansion and the presence of hair follicles make scalp reconstruction complex and difficult [4,5]. Several studies have proposed suitable reconstruction options according to defect size, defect location, radiation history, and hairline distortion, as well as algorithms to select them. Surgeons should utilize the simplest reconstruction method to achieve the most functional and aesthetic scalp reconstruction with minimal complexity [1,3].
Primary closure should be considered first for scalp defect reconstruction. However, in vivo studies have shown that the scalp skin requires approximately three times more force to induce a given stretch than does the skin on the back of the hand or abdomen, as the scalp is less elastic, particularly because of the galea aponeurosis. It has also been suggested that a scalp wound should not be closed when a force of 15 N or more is required for wound edge approximation, due to the risk of stitches penetrating the skin and blood flow disturbance [7,8]. In previous studies investigating scalp reconstruction algorithms, reconstruction was performed through primary closure only for small (<10 cm2) defects that occurred in the loose scalp (i.e., the temporal/temporoparietal and lateral occipital areas), and subgaleal undermining or galeotomy was performed for tension-free closure [1,3,4,9].
Galeotomies have been used not only in various reconstruction approaches such as primary closure, local flap, and tissue expansion, but also in cosmetic surgery procedures such as hairline lowering surgery [10,11]. Previous biomechanical studies have shown the eventual benefits provided by galeotomies such as wound tension reduction and scalp advancement. Raposio et al. [12] have revealed the effectiveness of galeotomies, finding only a slight improvement in flap advancement ability (1.67 mm per galeal incision), but a significant (40%) reduction in wound tension. Tyrell et al. [13] have demonstrated that five serial galeotomies with an average flap advancement of 2.56 mm per galeotomy increased the overall flap advancement by 85%. This decrease in tension may lead to fewer wound healing complications.
In the present study, the defects were medium-sized with a mean area of 12.6 cm2 (range, 7–24 cm2), and the defect was located in the tight zone in eight cases. According to scalp reconstruction algorithms, a local or regional flap was required to reconstruct the defects in our study. However, since local or regional flaps must be rather large to cover even relatively small defects, surgery becomes complex and time-consuming. This can potentially result in complications such as blood loss, reduced sensation, altered hair growth and even skin necrosis [7,8]. Therefore, we performed primary closure, the simplest reconstruction method, and used galeotomies to reduce wound tension.
Ideally, galeal scoring incision lines to increase flap length should be placed perpendicular to the maximum tension line. Moreover, the first galeotomy incision should be at least 1 cm away from the wound edge to prevent the galea from tearing when sutured. Each galeotomy incision should be spaced 1 cm apart, and the incision should be examined after each scoring to ensure proper tissue length [3-5]. Importantly, it should be noted that the galea is a thin layer, and to reduce the risk of excessive bleeding, galeotomies should be performed under direct vision. In most studies, galeotomies were performed after large incisions and extensive flap elevation [5,10,11].
Wide flap elevation allows easy lifting of the skin, ensuring good exposure of the undersurface to facilitate galeotomies. Conversely, flap elevation through a small incision provides insufficient space for performing galeotomies. With insufficient flap elevation, the blade has to approach the underside of the flap at an angle. The farther away from the wound edge the blade reaches, the more obliquely it comes into contact with the undersurface, rendering elaborate incisions difficult to make. Moreover, it is difficult to determine whether the galeotomy was performed in the accurate location and at the appropriate depth when the surgical field of view is narrow. We were able to make the edge of the blade face up by holding on to the hole in the middle of the no. 15 blade with mosquito forceps. As a result, the blade could enter through the narrow opening of the incision to reach the flap’s undersurface vertically without tilting, incising the tissue effectively. After each galeotomy, we elevated the flap as much as possible to check that the incision was made in the appropriate location and at the appropriate depth without any bleeding.
Performing a surgical procedure with a small incision and narrow surgical field is difficult. In dentistry, instruments with an adjustable scalpel handle that can adjust the angle of the scalpel blade are sometimes used. Fogli [14] reported a method wherein blunt-tipped, curved scissors were inserted through a hairline incision during galeal incision in the temporal area. In our study, we performed galeotomy by utilizing a simple method fixing a no. 15 blade using mosquito forceps. As a common and familiar tool, mosquito forceps have the advantage of being immediately useable in surgery, without the need to purchase or practice using new tools.
This study has several limitations. First, if performed by an inexperienced surgeon, the surgical technique used in this study could make it difficult to secure the surgical field, raising the risk of damaging vessels overlying the galea which could lead to complications such as bleeding and hematoma. Supplementing the technique with endoscopic assistance or loupe magnification could improve these aspects. Second, the retrospective design of this study resulted in inadequate data collection and potential information bias. There was also a possibility of recall bias in the telephone interviews. Third, because of the relatively small sample size and differing defect locations and sizes, statistically meaningful comparisons with other studies were not possible. Last, deep scalp defect cases with cranial bone exposure were not included. Reconstruction of severe defects with exposure of the cranial bone can be more complex and challenging, and it is necessary to investigate whether our proposed technique can be applied to these cases. Despite these limitations, our study can help surgeons select pre- and intraoperative reconstruction methods.
In conclusion, the present study suggests that galeotomies can be successfully performed, even in a restricted space, by using mosquito forceps. Thus, the simplest reconstruction method can provide the most functional and aesthetic scalp reconstruction with minimal complexity. Through our proposed method, medium-sized defects could be reconstructed relatively easily and safely in a short amount of time, and satisfactory results could be achieved without complications.
Notes
No potential conflict of interest relevant to this article was reported.


