Dual Application of Mesh through Hybrid Technique in Large Incisional Hernia: A Case Report
Article information
Abstract
Although single mesh insertion is recommended for simple incisional hernia, there is no established treatment of choice for severe incisional hernia accompanied with large muscular defects. Single mesh insertion cannot provide sufficient mechanical force, and muscle flaps could lead to donor site morbidity while also requiring longer operation times. In this case, dual application of mesh through a hybrid technique could be a good option. A 46-year-old woman with rectus abdominis muscle defect due to previous surgery visited our clinic with abdominal bulging. Abdomen-pelvis computed tomography demonstrated a 6.5×11.5 cm rectus abdominis defect along with small bowel herniation. We decided to reinforce the existing hybrid intraperitoneal onlay mesh technique through additional insertion of suprafascial mesh to prevent recurrence and minimize complications. The patient’s abdominal contour was well preserved postoperatively for 1 year. We believe dual-layer mesh insertion through a hybrid approach could be a better alternative for severe incisional hernia with large muscle defects because of its treatment efficacy, short operation time, simple technical requirements, and absence of donor or flap complications.
Introduction
Incisional hernia can occur after any abdominal surgical procedure in which the abdominal wall is incised. Although small and asymptomatic hernias can be managed with conservative care, surgical repair is required for large or symptomatic hernias to relieve symptoms and prevent further complications. In case of hernias requiring surgical treatment, it is currently recommended to use a mesh for additional reinforcement in hernias >1 cm in diameter, along with primary closure of the fascial defect [1]. The mesh could be inserted at various layers, and guidelines recommend the intraperitoneal onlay mesh (IPOM) method as one of the best options for repair of incisional hernia [1].
Several studies have reported cases using the hybrid IPOM method in which suprafascial and laparoscopic approaches are both used. This approach has been proved to be safe and effective for large and complex incisional hernias, since the open approach is associated with less technical difficulty during extensive adhesiolysis and redundant tissue excision. These procedures can be difficult to manage through laparoscopy due to the increased risk of intraoperative or postoperative complications such as enterotomy or seroma. However, the hybrid IPOM method still has its limitations in cases of incisional hernia with large muscle defects, with recurrence rates reported up to 6%–12% [2,3]. The recurrence rate increases as the muscle defect becomes larger, which makes it difficult for single-layer mesh insertion to provide adequate mechanical force for long term-support of the herniated visceral contents. Muscle flaps have been suggested to solve this issue, but flap surgeries are inevitably accompanied by complications such as donor site morbidity or flap necrosis. Therefore, we present a clinical case of dual-layer mesh insertion in both the suprafascial and intraperitoneal layers using a hybrid approach, which may be a better surgical option for severe incisional hernia with a large muscle defect. This approach is expected to have higher treatment efficacy and a lower recurrence rate compared to other existing methods such as the hybrid IPOM method or muscle flaps.
The report was approved by the Institutional Review Board of Seoul National University Hospital (No. H-2206-154-1335). Informed consent has been obtained for this publication from the patient.
Case
A 46-year-old woman with a body mass index of 25.30 kg/m2 visited the clinic because of a left lower abdomen bulge which started 1 month prior (Fig. 1A). She had undergone a cesarean section with a Pfannenstiel incision 20 years ago and uterine high-intensity focused ultrasound (HIFU) therapy to treat a uterine myoma 2 years ago. She had also subsequently received an open myomectomy 1 year after the previous HIFU due to remnant myoma. Partial necrosis of the left rectus abdominis muscle was identified during the myomectomy, probably due to the thermal injury caused by HIFU at the anterior abdominal wall muscles. Although she showed no symptoms right after the myomectomy, the left lower abdomen started to bulge gradually after 1 year. This was accompanied by severe pain which was induced even by low-intensity exercises such as jogging. Physical examination revealed abdominal bulging above the left side of the previous cesarean section scar. Contrast-enhanced abdomen-pelvis computed tomography revealed a small bowel herniation through a 6.5×11.5 cm rectus abdominis defect. There were no signs of bowel strangulation or incarceration (Fig. 2A). Considering the extensive loss of muscle, we planned to use dual-layer mesh reinforcement through a hybrid approach.

Medical photo of the patient. (A) Medical photo before hernia repair. (B) Medical photo 6 months after hernia repair.

Abdomen-pelvis computed tomography (APCT) imaging. (A) APCT before surgery showed a 6.5×11.5 cm rectus abdominis defect along with small bowel herniation. (B) APCT 6 months after the surgery showed intact intraperitoneal onlay mesh (yellow arrow) and suprafascial mesh (blue arrow).
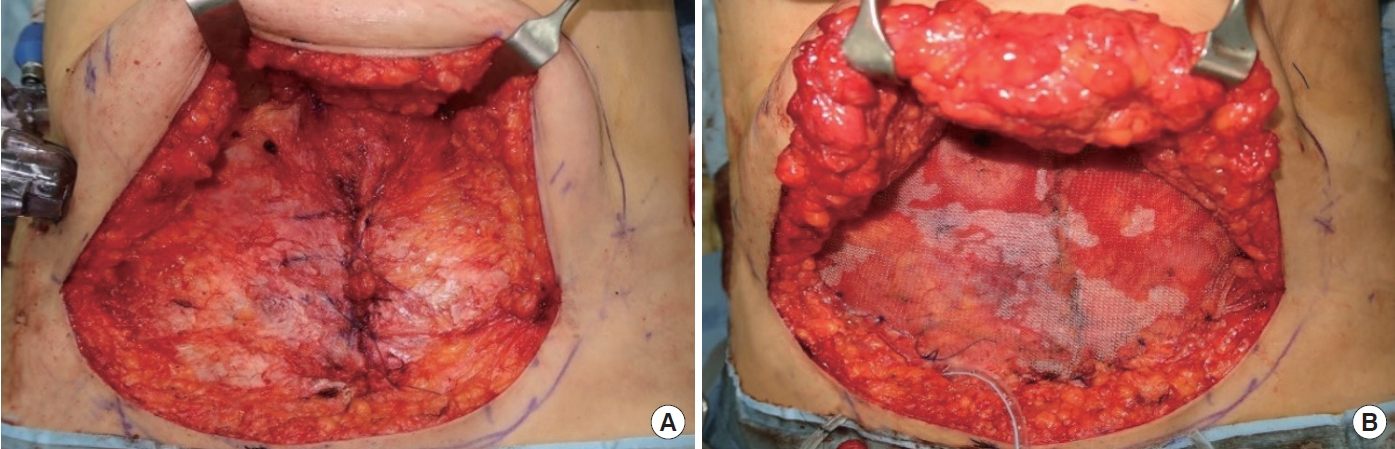
Surgery was performed under general anesthesia without the concurrent use of epidural anesthesia. A Veress needle was inserted into the left upper quadrant, and CO2 insufflation was performed. A 12-mm camera port and two 5-mm additional ports were inserted (Fig. 3A), followed by peritoneal exploration and hernial sac identification. The surgery proceeded in the following four steps: first, mild adhesions were found between the omentum and abdominal wall, followed by adhesiolysis. After CO2 exsufflation, a 20-cm-sized transverse skin incision was made along the previous cesarean section scar (Fig. 3A), followed by suprafascial dissection. Second, anterior rectus fascia plication was performed through a purse-string suture with 2-0 Vicryl and 1-0 Prolene followed by interlocking sutures with 1-0 Prolene (Fig. 4A). Third, after CO2 re-insufflation, the surgeons applied an IPOM over the hernia site using a 12×12 cm composite mesh (Symbotex; Medtronic) coated with collagen to prevent adhesions. The mesh was applied to overlap the hernia orifice by at least 3 cm (Fig. 3B). Transfascial sutures were made in four quadrants and fixed with a surgical tack (CapSure; Becton Dickinson). Finally, following CO2 re-exsufflation and further suprafascial dissection, a trimmed Prolene mesh (Bard; Becton Dickinson) was applied over the anterior rectus fascia. The mesh was secured to the fascia by simple sutures using Prolene 1-0 (Fig. 4B). At the suprafascial space, one Hemovac drain was inserted followed by application of fibrin sealant. The wound was closed layer by layer, with the total operating time measured as 240 minutes. The patient was discharged on postoperative day 7 and wore an abdominal belt for 6 months. Computed tomography performed 6 months postoperatively showed no signs of recurrence and no migration of either mesh (Figs. 1B, 2B).

Intraoperative photo. (A) Operation schema showing the location of the laparoscopic port and skin incision for suprafascial approach. (B) Intraperitoneal onlay mesh insertion through a laparoscopic approach.
Discussion
The present case is notable in terms of the patient’s extensive rectus abdominis defect caused by postoperative muscle necrosis. In this case, single-layer mesh insertion through the hybrid method could not provide sufficient mechanical force for long-term support of the herniated visceral contents. Although abdominal wall reinforcement using a pedicled muscle flap has been reported in previous studies, it has disadvantages such as donor site morbidity, high technical requirements, and muscle flap necrosis or atrophy [4]. Therefore, we hypothesize that reinforcement of the existing hybrid IPOM method through additional suprafascial mesh application could be a reasonable option for severe incisional hernia in terms of lowering the recurrence rate and complications, and promoting treatment efficacy at the same time.
The use of a mesh which could be inserted at various layers has been recommended for hernias >1 cm due to high recurrence rates. Onlay mesh placement is relatively easy to perform but there is a higher risk of skin denervation and necrosis due to extensive subcutaneous dissection. The sublay method requires a relatively long operative time but is currently preferred by many surgeons due to minimal postoperative adhesions. The IPOM method is preferred for its mechanical stability, especially when the fascia or muscle defect is large or there is constant significant pressure caused by herniated viscera. In fact, according to current guidelines, the IPOM method is recommended as one of the best options for repair of incisional hernia. However, open IPOM requires extensive dissection along the pre- and retro-muscular space, and therefore increases the possibility of postoperative seroma, hematoma, or pain. Laparoscopic IPOM is associated with the risk of enterotomy, and it is also difficult to perform extensive adhesiolysis. These limitations led to the development of the hybrid IPOM method, in which both suprafascial and laparoscopic approaches are utilized [3,5]. Although the hybrid IPOM method is currently widely used for incisional hernia, severe incisional hernia still has a relatively high recurrence rate up to 6%–12% [2,3]. Our case was a severe one in terms of the large muscle defect, measured as 6.5×11.5 cm, and we therefore anticipated that a single mesh could not provide sufficient mechanical force. For this reason we decided to reinforce the existing hybrid IPOM method with additional suprafascial mesh insertion to achieve greater rigidity of the abdominal wall and lower the recurrence rate.
In this case, a severe incisional hernia with a large muscle defect was successfully managed with a dual-layer mesh application through a hybrid approach. We believe that the dual mesh can provide stronger abdominal wall reinforcement and lower the recurrence rate compared to the previous hybrid IPOM method. The patient’s abdominal contour was well preserved postoperatively for 1 year, despite the initial extensive muscle loss. Further studies are required for a more thorough evaluation of our proposed method.
Notes
No potential conflict of interest relevant to this article was reported.