Introduction
Pilonidal sinus disease occurs with a frequency of 0% to 5% in the general population. It presents as a cystic lesion or draining sinus tract involving the sacrococcygeal area [1]. A chronic form gives rise to intermittent discharge from the sinus tract [2,3]. In rare cases, a long-standing pilonidal sinus can lead to malignant transformation of the sinus tract and overlying skin, eventually leading to squamous cell cancer (SCC) [4]. This rare complication is observed mainly in chronic, recurrent, and untreated primary pilonidal disease. The incidence of malignant change occurs in approximately 0.1% of patients with pilonidal disease, mostly in males. According to previous studies, the mean duration of pilonidal sinus disease that leads to squamous cell carcinoma is over 20 years [4,5].
Herein, we present a rare case of malignant transformation of a pilonidal cyst in a relatively short time period. An unexpected squamous cell carcinoma was reported after surgical excision and biopsy to treat the original pilonidal cyst. Since the primary surgery plan was to remove only the pilonidal cyst, wide excision had not been considered. Part of the underlying squamous cell carcinoma remained, and an unhealed sinus tract caused a chronic open wound. Although the following treatment process was complicated, our reconstruction process for this chronic open wound can provide useful information for managing comparable cases.
This report was approved by the Institutional Review Board of Konkuk University Hospital (IRB No. KUH 2022-10-054) and written informed consent was obtained from the patient.
Case
A 56-year-old female patient visited the general surgery department of our hospital with a slowly growing palpable mass in the coccyx area. The lesion had appeared 2 years prior after a traumatic contusion caused by a fall-down accident. Aspiration had been performed to relieve the bulging area several times at a local health clinic, which had yielded a yellowish serous fluid. The bulging area decreased temporarily after each aspiration session, however the lesion relapsed in a few days. The local clinic had not done any bacterial culture or liquid analysis tests of the aspirated fluid. Otherwise, the patient had no medical or surgical history; however, she had also previously sustained another traumatic contusion in the same area, again caused by a fall-down accident, 7 years prior to her presenting to our hospital. Magnetic resonance imaging (MRI) revealed a 17-cm retrococcygeal cystic mass at the subcutaneous layer with thin wall enhancement. The radiologist’s report of the preoperative image was a pilonidal cyst with a partially mixed solid portion (Fig. 1A and B).
The general surgeons planned for primary excision of the coccygeal pilonidal cyst, which was performed through a transverse oval-shaped (8×4.5 cm) incision. Careful dissection was conducted extending deep into the retrorectal space, and a 20-cm cystic mass containing dark brown fluid and severely adhered to the vicinity was removed. The solid portion (1.7×1.0 cm) adjacent to the skin layer was also removed. Primary closure was performed to repair the incisional wound because the surgeons considered the resection thorough enough and the cystic mass to be a benign lesion. Permanent biopsy of the specimen obtained revealed moderately differentiated SCC with involvement in the resection margin of the solid tumor portion (Fig. 1C), and no lymphovascular or perineural invasion. The pathologist commented that a partial layer of the original pilonidal cyst might have transformed into malignant SCC in the adjacent area.
Since the presence of SCC was determined, the general surgeons postponed any additional surgical procedures until a full malignancy work-up. Positron emission tomography, abdomen-pelvic computed tomography (CT), neck MRI, sigmoidoscopy, and uterine ultrasonography revealed no metastatic lesions. After excluding hidden malignancies or metastasis, the general surgeons decided against additional excision since successful wound closure was not expected to be possible. During postoperative wound management, serous discharge constantly increased, and dehiscence occurred at the incision repair site. The skin and soft tissue around the wound margins showed signs of infection, including redness and swelling. Swab cultures of the wound site identified Klebsiella pneumonia for which ampicillin/sulbactam was administered intravenously. This infection led to the delay of other treatments. Two months after the initial surgery, the signs of infection decreased. The general surgeons maintained conservative management with betadine dressings to induce secondary intention healing of the remaining wound. However, for the following month the 2.5×1.5 cm sized open wound did not display normal signs of a healing process.
The patient was subsequently transferred to the department of plastic and reconstructive surgery for management of the unhealed coccygeal wound. When the patient visited our clinic, the wound had a 1.5×0.5 cm sized round opening and displayed minimal discharge without infection signs (Fig. 2A and B). Additional wound swab cultures showed no pathogen growth. Although the wound opening had decreased in size, contrast-enhanced CT still showed an open wound connected to an underlying cyst with free air (Fig. 2C and D). Cyst pocket undermining subcutaneously extended more than 3 cm from the wound opening in cephalad, caudal, and bilateral directions (Fig. 3A).
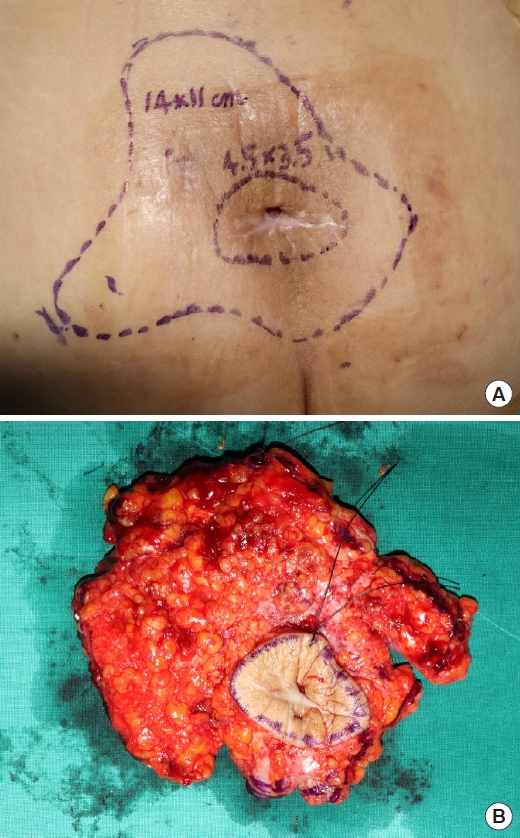
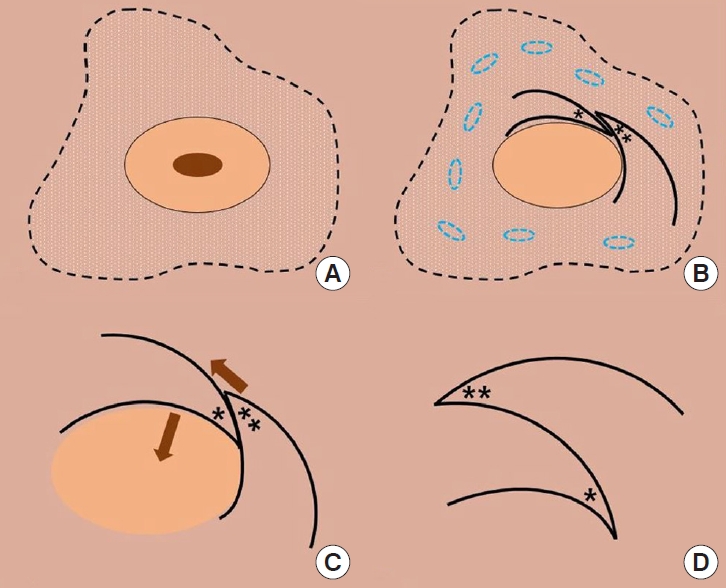
The cause of the nonhealing state was presumed to be related to residual tumor or a draining sinus tract. Therefore, we planned additional wide excision of the skin around the opening and underlying cyst in the subcutaneous layer. We conducted a thorough resection of the periwound skin with a wide margin (1.5 cm). The cyst was also dissected including mucosal tissue forming a pocket around the coccyx (Fig. 3B). The surface area of the skin defect after excision was 4.5×3.5 cm, and the underlying tissue defect consisted of a 14×11 cm sized subcutaneous pocket reaching the supra-fascial layer with the gluteal fascia exposed. After confirming a clear resection margin by frozen biopsy, we designed two triangular skin flaps based on adjacent perforators and used them for coverage of the open wound and cavity (Fig. 4).
In the postoperative period, the patient alternated between prone and lateral positions to prevent excessive pressure on the coccyx area and Jackson-Pratt drain site. Additional fluid collection or wound discharge was not noted on postoperative CT images (Fig. 5A and B). The final biopsy results reported moderately differentiated SCC with a clear resection margin and no lymphovascular or perineural invasion (Fig. 5C). After 3 weeks, the wound healed without complications, and the patient was discharged. The patient returned to regular daily activities after a 1-month healing period, and the healed site remained stable without dehiscence or recurrence at the 6-month follow-up visit (Fig. 6). Light exercises, including walking and sitting, were possible without difficulty.
Discussion
A pilonidal cyst can progress to a chronic lesion, with various factors associated with the pathogenesis. de Parades et al. [1] demonstrated the leading causes of healing failure in a pilonidal sinus. Prolonged infection, the persistence of multiple pits, bacterial super-infection, subcutaneous walling-off, excessive hair growth, and wound dehiscence showed a causal relationship. Mayol Oltra et al. [4] pointed out the pathogenesis of malignant degeneration, in which the main course was similar to other chronic cutaneous disorders. Aberrant release of free oxygen radicals can induce genetic damage and lead to neoplastic transformation. Additionally, the standard DNA repair mechanism is impaired in chronic inflammation which predisposes patients to malignancy. The process of malignant transformation can be aggravated by other conditions, such as burns, scars, skin ulceration, and fistulas. In our patient, the estimated period of malignant transformation was shorter than in previous case reports. We assume that the repeated aspiration history before initial surgery could have led to mechanical and chemical trauma to the adjacent skin and soft tissues.
The wound healing process generally consists of the hemostasis, inflammation, proliferation, and remodeling phases [6]. The natural course of the healing process takes place in a cascade, and the necessary factors and resources appear and regress sequentially. The process can be hindered by innate disease or external disturbances. Underlying clinical conditions, including diabetes mellitus or autoimmune disease, and patient factors, such as alcohol or tobacco usage and excessive pressure, are common causes of delayed wound healing. In our patient, bacterial wound infection and residual malignant lesion contributed to the chronic open wound [7,8]. Incomplete resection of the pilonidal disease could have added another causality. Nonetheless, a strategic approach led to curative treatment and adequate wound closure.
The probability of epidermal or pilonidal cysts spontaneously progressing into malignancies is considerably low. Even in cases of chronic infected pilonidal cysts, the risk of developing SCC can be reduced by appropriate initial treatment [5]. In our patient’s case, preoperative imaging studies failed to help predict the presence of SCC before the initial surgery; residual SCC was discovered only through postoperative pathology tests.
Our surgical team decided to perform radical removal of the causative structures (i.e., overlying skin, cyst wall, surrounding subcutaneous fat, and connective tissues) and reconstructed the chronic open wound in the coccygeal area [9]. When managing skin malignancies, thorough resection of the lesion with an adequate safety margin including adjacent tissue is crucial [10]. The surgical principle of en bloc resection was sustained throughout the entire sequence. With regard to the reconstruction, a quilting suture technique was implemented at multiple sites to prevent additional fluid collection in the postoperative period [11]. Thereafter, two triangular flaps, one transposition flap and one advancement flap, were utilized to fill the 4.5×3.5-cm skin and soft tissue defect [12]. Both flaps were elevated including skin and subcutaneous layers for sufficient coverage of the gluteal fascia [13]. Adequate relocation of the flaps resulted in effective restoration, avoiding excessive tension on the margins.
The limitation of this care report is the short follow-up period. The patient was monitored for 6 months, during which no adverse events occurred. However, the limited follow-up can raise concerns regarding seroma formation and cancer recurrence. The patient’s condition will be continuously checked every 3 months, using careful physical examination and imaging studies.
In summary, a pilonidal sinus appeared after traumatic contusions, and the lesion progressed to malignant SCC. The short period for malignant transformation is notable, and mechanical and chemical injuries could have contributed to tissue alteration [7]. Imaging studies before the primary excision seemed to display a benign pilonidal cyst. However, the postoperative pathologic report demonstrated SCC in the solid portion. Surgeons should consider the possibility of malignant transformation when planning management of a chronic wound [14].