Introduction
Nontuberculous mycobacterium (NTM) are species of the genus Mycobacterium not including Mycobacterium tuberculosis and Mycobacterium leprae. NTM are frequently present in the environment, such as in soil, tap water, swimming pools, and animal reservoirs.
The incidence of NTM infections is increasing worldwide [1,2]. While pulmonary diseases are the most common illnesses caused by NTM infection, approximately 20% to 30% of NTM infections cause extrapulmonary diseases such as those involving the musculoskeletal system and soft tissues [3,4]. The hand and wrist are the most common sites of musculoskeletal NTM infection.
If treatment for musculoskeletal NTM infections is delayed, the infected tissue can be damaged by caseous necrosis, eventually leading to serious sequelae [5]. Furthermore, NTM infections tend to recur, and extensive debridement may be required, often leaving a large defect.
A few cases of NTM infection of the hand have been reported [6–9]. However, none of the patients underwent reconstruction for soft tissue defects caused by NTM infection and debridement. We herein present a rare case where an NTM infection of the hand led to soft tissue defects and was treated with antibiotics and well-vascularized flap coverage. The patient provided written informed consent for the publication and the use of his images.
Case
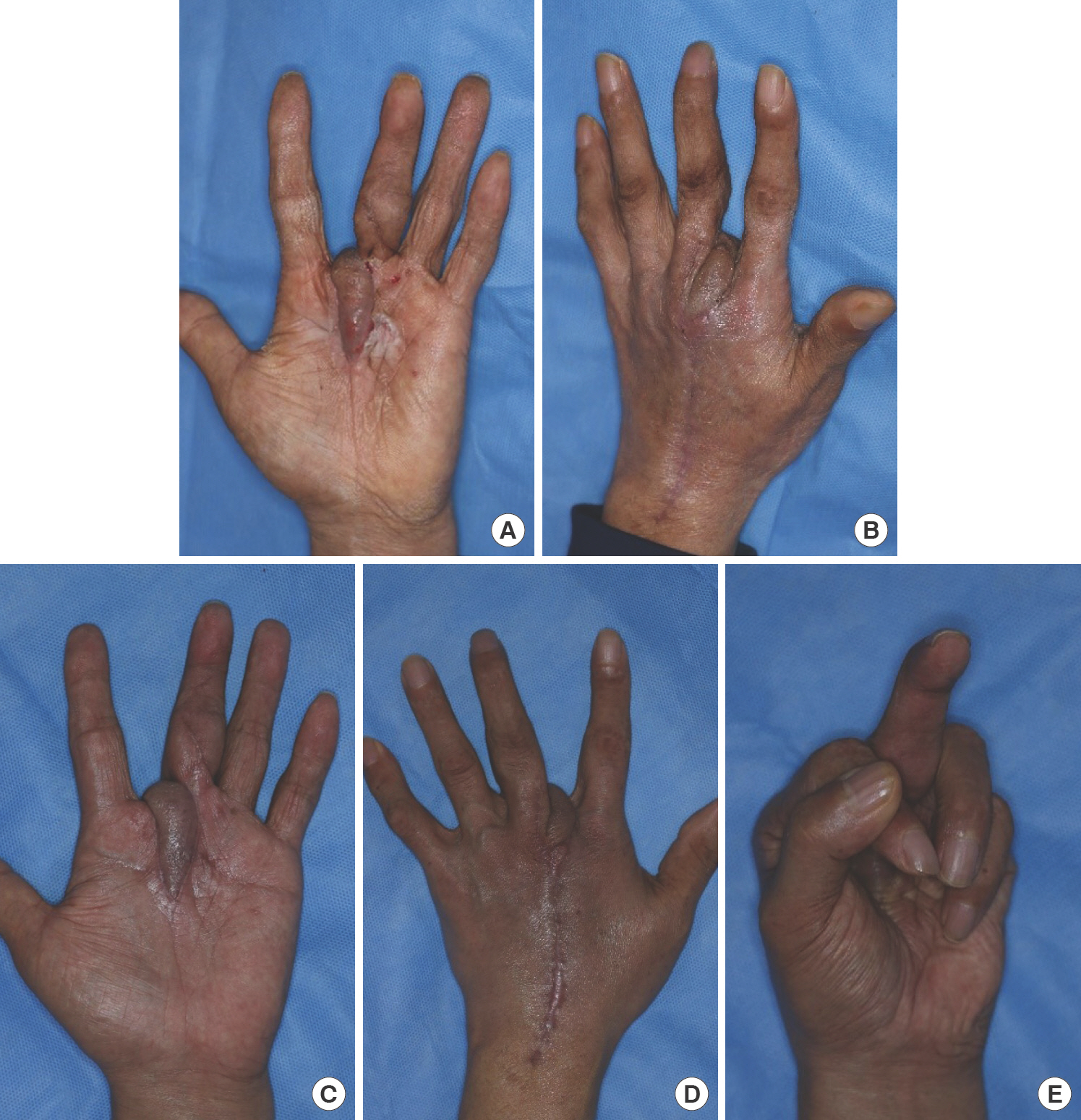
A 56-year-old man with a medical history of diabetes arrived from another hospital with a painful chronic wound on the palmar side of the third metacarpophalangeal joint area and in the second web space of the left hand (Fig. 1A and B). A large amount of callus was formed on the palmar side, and a small amount of purulent discharge was oozing from the wound in the second web space.
Fig. 1.
Initial wound and intraoperative images of synovectomy and pulley reconstruction. (A) Initial wound on the palmar side. (B) Initial wound on the second web space. (C) Incision made by orthopedic surgeons. (D) Synovectomy, tenolysis, and preparing pulley reconstruction.
He was initially admitted for trigger finger and was diag-nosed with chronic tenosynovitis in the other hospital. He was treated several times with steroid injections for 4 months, but eventually an infection occurred at the injection site. The patient underwent incision and drainage of the infection site and three debridement procedures in that hospital. Despite antibiotic administration and surgical intervention, the wound did not heal. He visited our institution for a second opinion 3 months after the first incision and drainage procedure.
The patient had severely limited range of flexion on the metacarpophalangeal, proximal interphalangeal, and distal interphalangeal joints of the right middle finger. Our hospital's orthopedic surgeon planned synovectomy to manage recur-rent inflammation and A2 pulley reconstruction to replace the A2 pulley that had “melted down” due to the enduring infection (Fig. 1C and D). A tissue biopsy was performed during surgery, and the specimen was analyzed by hematoxylin and eosin staining, Gram staining, and culture. The results were negative for bacteria and fungi, and the pathology results sug-gested chronic non-specific inflammation.
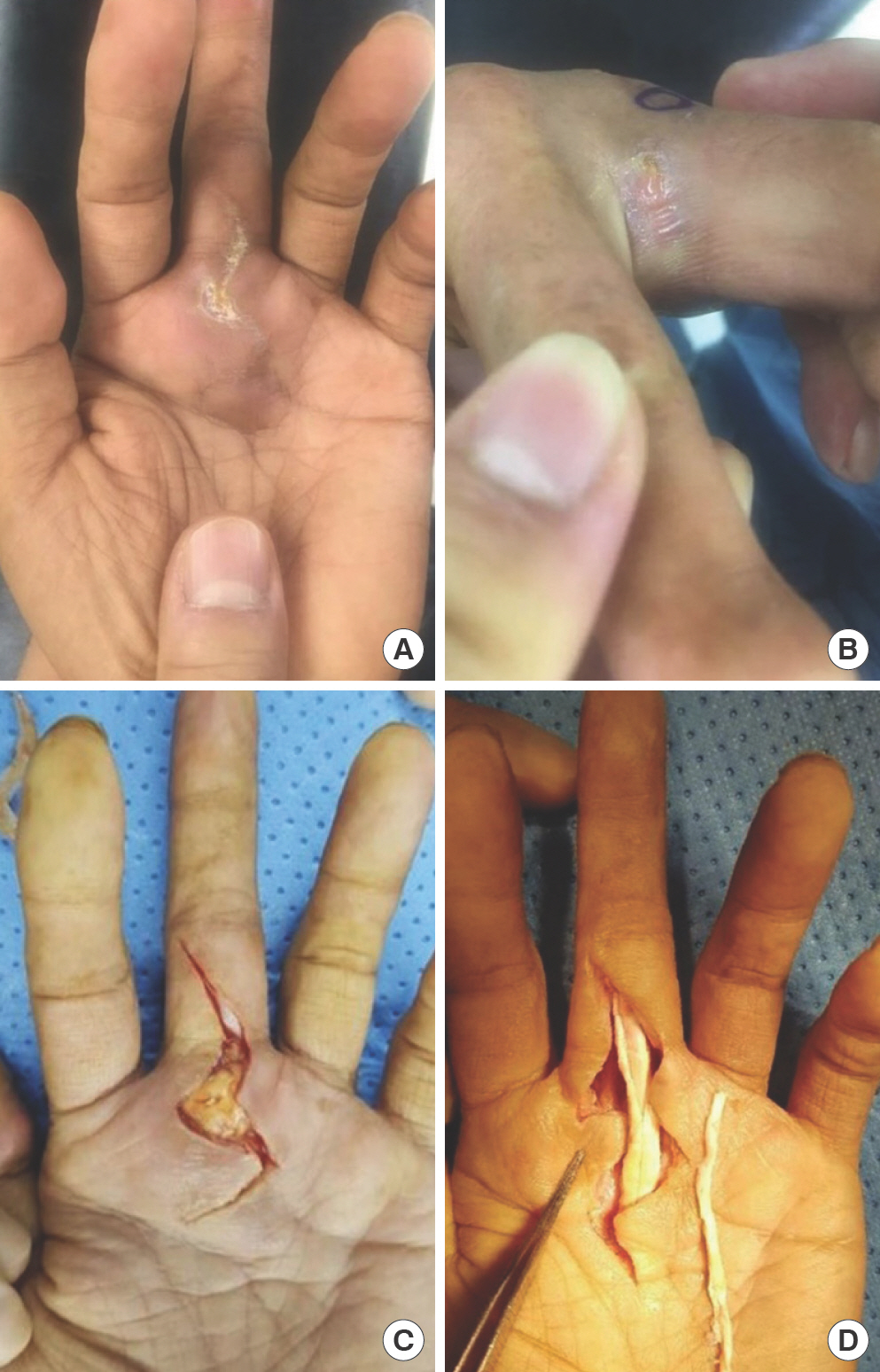
Despite the surgery, the operation site continued to undergo necrotic changes. Thus, magnetic resonance imaging (MRI) was performed, revealing heterogeneous high signal intensities and an atypical enhancement pattern, suggesting chronic sy-novitis, potentially with tuberculosis (Fig. 2). NTM were cultured in acid-fast bacilli liquid culture after wound culture was repeated. Acid-fast staining and polymerase chain reaction results were negative for NTM, but acid-fast bacilli liquid culture revealed Mycobacterium marinum and Mycobacterium ulcerans. Pathology findings confirmed the presence of chronic granulomatous inflammation with necrosis, indicating an atypical mycobacterial infection. The patient received clar-ithromycin 500 mg (twice a day), ciprofloxacin 750 mg (once a day), doxycycline 100 mg (twice a day) for 5 months, and in-tramuscular amikacin 500 mg (three times a day) for 1 month, in accordance with drug susceptibility results. As no oral amikacin agent was available, administration was performed only during the patient's hospitalization period.
Fig. 2.
Three months after pulley reconstruction. (A) Nodular lesion with focal ulceration suggestive of nontuberculous mycobacterium infection. (B) Magnetic resonance imaging showing an atypical enhancement pattern.

However, the surgical site continued to undergo necrotic changes; thus, 3 months after the synovectomy and pulley reconstruction, the orthopedic surgeon referred the patient to the department of plastic surgery for soft tissue coverage after radical debridement of the inflamed tissue.
After due consideration, we decided to use a second dorsal metacarpal artery flap (DMAF) for wound coverage. The second DMAF could cover the dorsal and proximal palmar side of each finger. Furthermore, because the infection was on the palmar side and the web space, the second DMAF was pre-ferred, as it could be elevated from the dorsal side. Moreover, considering that a thick flap may obstruct functional finger movement, the DMAF also had the advantage of thin flap ele-vation.
Nearly 4 months after the pulley reconstruction, we performed synovectomy and debridement together with an orthopedic surgeon. Flap coverage was performed 10 days after the synovectomy and debridement. During surgery, we performed additional debridement of the infected tissue. A 3×5-cm defect was created on the palm and second web space owing to the debridement. The arterial system of the hand was intact, with abnormality detected by three-dimensional (3D) angiographic computed tomography of the upper extremity. The second DMAF, measuring 3×12 cm, was elevated. The flap was transposed to cover the defect and sutured with 5-0 nylon. The flap donor site on the dorsum of the hand was closed by primary repair. Immediate postoperative observation revealed that the distal part of the flap had a normal capil-lary refill time, i.e., approximately 2 to 3 seconds (Fig. 3). The patient was transferred to a general ward where the refill, col-or, and arterial pulse were monitored every 2 hours for 3 days. On a postoperative day 2, venous congestion occurred (Fig. 4). The flap was salvaged using a total of 20 medicinal leeches at 3-hour intervals. During the intervals between leech application, continuous bleeding was induced by applying heparin-soaked gauze to the bleeding site. After successful flap salvage, the patient was discharged with no other postoperative com-plications. At the 3-month follow-up after DMAF reconstruction, the wound had healed with no evidence of infection recurrence. Metacarpophalangeal joint flexion became nearly normal, but proximal interphalangeal joint flexion was limited as it was when the patient first visited our hospital (Fig. 5).
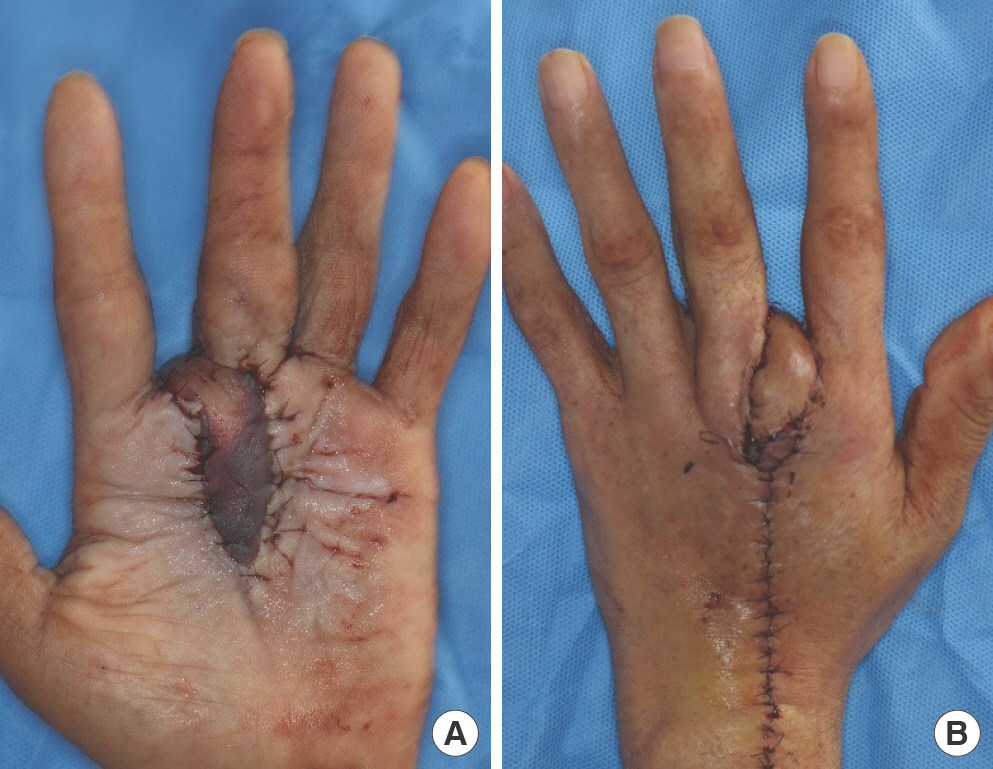
Fig. 3.
Immediate postoperative image of flap coverage. A 3×12-cm second dorsal metacarpal artery-based flap is elevated from the dorsum of the hand. Flap transposition is performed. (A) Palmar view. (B) Dorsal view.

Discussion
When planning treatment for a chronic wound with no signs of healing despite long-term conventional treatment, wound infection, caused by fungi, bacteria, or viruses, should be considered as part of the diagnosis. NTM infection is particularly frequently overlooked because it is difficult to detect with conventional bacterial culture, and the symptoms are often mild. In this regard, NTM infections should be granted more attention.
Soft tissue or musculoskeletal NTM infections can occur when pathogens enter the skin through wounds. In our patient, M. marinum and M. ulcerans were identified. The source of infection of both strains is known to be related to aquatic environments. M. marinum is both found in fresh and salt wa-ter; people may become infected while fishing. M. ulcerans infection is common around swamp areas [5]. Our patient worked in a junkyard, which contained a collection of various wastes, possibly contaminated with NTM. Therefore, he may have been infected with Mycobacterium in the garbage (e.g., fishing hooks) through the wound in his hand.
The patient in this case, had one suspected risk factor in ad-dition to the occupational risk of exposure to NTM. He had chronic tenosynovitis, for which he had received long-term steroid injections. NTM infection due to intra-articular injections such as steroids have been reported previously. The prob-able reasons for this are contamination with NTM during the injection process and the affected area becoming vulnerable to infection due to triamcinolone [10,11].
The clinical features of M. ulcerans infection include papules or ulcerative nodules as well as necrosis of adipose tissue, a condition called Buruli ulcer. A large number of M. ulcerans surround the ulcerative lesion around the necrosis. For all patients with suspected Buruli ulcers, specimens should be sent for pathology and for laboratory tests, and the patient should be treated under direct observation for 8 weeks with the rec-ommended combination of rifampicin and streptomycin or rifampicin with another oral antibiotic agent. A standard antibiotic regimen was established by the World Health Organization, but other antituberculosis medications can be used alter-natively, depending on drug susceptibility.
Musculoskeletal NTM infections often require simultane-ous treatment with antibiotics and surgery. Even with appropriate antibiotics and surgical treatment, the infection may recur and require continuous debridement [3,5,12]. Multidisci-plinary treatment should be considered if the wound is infected with NTM. To localize the infected lesion, imaging tests including MRI may be necessary, and close consultation with infectious medicine is required to maintain proper antibiotic treatment. In this case, the three most important factors of NTM infection treatment were infection control with antibiotics, debridement of the infected tissue, and coverage with a well-vascularized flap.
The hand is an intricate part of the body which function has not only physical but also social, aesthetic, and psychological components. Soft tissue defects or necrosis due to trauma, burns, and tumor resection can lead to permanent damage to various functions of the hand if not properly treated. Tissue loss is one of the most important factors to be considered when selecting methods to cover defects, the other significant factors being defect size, site, depth, orientation, and composition.
The DMAF is one of the most effective techniques for reconstruction of hand defects. In 1987, Earley and Milner [13] first introduced the proximal DMAF based on the first and second dorsal metacarpal arteries. The DMAF was conventionally used to manage thumb defects, but it is also used to cover palmar surface defects. The second DMAF can cover the proximal palmar and nearly the entire dorsal surface of the fingers [14]. With recent advancements in microsurgery, free flap transfer can be an attractive alternative; however, it is a rather complicated choice that may be the second option depending on the operating institution and the surgeon's prefer-ence.
In this case, using the second DMAF in NTM infection had the advantages elevating a flap far from the infection site and achieving single-stage coverage in through a flap with robust blood supply. The 3D volume of the DMAF on the palmar surface is relatively small, especially when elevated as a thin flap, thus reducing the risk of obstructing finger movement. It is also aesthetically acceptable and has the advantage of a short operation time [14]. Although venous congestion is a major potential complication of the reverse DMAF like most other distal reverse flow flaps, salvage of the flap from venous congestion was successfully performed by leech therapy and with heparin-soaked gauze application in this case [15].
In previously reported NTM infections of the hands, infection was managed with medical treatment and wound dressings, and no patients underwent reconstruction of soft tissue defects from NTM infection and debridement [6–9]. Street et al. [6] reported seven cases of NTM infection of the hands but none of the cases required reconstructive surgery. Balague et al. [9] reported a case of NTM infection that eventually led to fifth finger amputation after serial debridement. We present a rare case in which NTM infection of the hand led to soft tissue defects, treated with a combination of antibiotic therapy, debridement, and coverage with a well-vascularized flap.