 |
 |

|
| Aims and Scope |
| About the Journal |
| About the Society (KWMS) |
| Editorial Board |
| Open Access |
| Principles of Transparency and Best Practice |
| Editorial Office |
| Subscriptions |


|
| Aims and Scope |
| About the Journal |
| About the Society (KWMS) |
| Editorial Board |
| Open Access |
| Principles of Transparency and Best Practice |
| Editorial Office |
| Subscriptions |

AbstractBackground Older patients with pressure sores secondary to medical problems generally are not likely to become physically active again and are therefore rarely considered candidates for flap surgery. When surgeons decide whether to perform surgery in older individuals with multiple morbidities, they must weigh the risks of prolonged general anesthesia and the burdens of flap surgery against the benefits of the flap.
Methods This retrospective study included patients over 65 years of age who were treated at our clinic from May 2010 to August 2018 for grade III or IV pressure sores. They underwent either general wound care without flap coverage (debridement only) or complete flap coverage of the sore (debridement plus flap group). We compared changes in laboratory blood tests from pre-operation to post-operation.
Results A total of 63 patients were included, with 53 in the flap coverage group and 10 in the control group. Age, sex, and flap size were statistically similar between groups (P>0.05). The control group exhibited no significant laboratory changes after debridement. The flap coverage group exhibited statistically significant improvements in neutrophil percentage and C-reactive protein level postoperatively (P<0.05, paired t-test). Serum hemoglobin, albumin and electrolyte levels did not differ with statistical significance from pre-operation to post-operation in either group (P>0.05, Wilcoxon signed-rank test and paired t-test).
IntroductionImproved living conditions and better medical care has significantly increased the life expectancy of older adults. With longer life expectancy, many older patients with multiple medical disorders require hospitalization. Poor mobility and a bedridden state secondary to age-related morbidities, including dementia and central nervous system injury, increase the risk of pressure sores. These sores interfere with normal nutrition, resulting in electrolyte abnormalities, and may increase the likelihood of infection, resulting in sepsis; without effective treatment, this can become a vicious cycle eventually leading to death [1]. Therefore, it is necessary to establish appropriate, early treatment of pressure sores.
General wound care for pressure sores includes debridement of necrotic tissue and the use of wound dressings and appropriate antibiotics. However, general wound care it is not always enough to cure pressure sores, and complete healing often requires debridement followed by myocutaneous or fasciocutaneous flap coverage [2]. Still, as older patients with multiple medical problems and pressure sores are not generally expected to resume much physical activity, they are rarely considered candidates for flap surgery. When surgeons decide whether to perform surgery in these patients, they must weigh the risks of prolonged general anesthesia and the burdens of flap surgery against the benefits of the flap. One advantage of flap surgery is that it has been reported to reduce septic shock-related factors, and debridement is known to reduce levels of inflammation in the body by removing dead and inflamed tissues [3]. The use of serum procalcitonin level as a predictor of successful surgical treatment of soft tissue infection is an example of utilizing these characteristics [4].
In this study, we compared the laboratory values before and after treatment of patients with infected grade III or IV pressure ulcers, who either had conservative treatment consisting of general wound care with debridement, or flap surgery with debridement as an active surgical intervention.
MethodsThis study was a retrospective comparative study. The study protocol was approved by Institutional Review Board of Kangnam Sacred Heart Hospital (IRB No. 2019-02-010). All procedures in the study involving human participants were performed in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The patients provided written informed consent for the publication and the use of their images.
This study included inpatients over 65 years of age who were cared for by members of the Department of Plastic and Reconstructive Surgery at our institution from May 2010 to August 2018. All patients had infected grade III or IV pressure sores, which were treated with either general wound care, including debridement of necrotic and infected tissue (the control group, debridement only), or debridement plus flap (gluteus maximus myocutaneous, posterior thigh, or tensor fascia lata myofasciocutaneous) coverage of the pressure sore (the flap coverage group). All patients in both groups were provided with intravenous antibiotics and adequate nutritional support, and their body position was changed every 2 hours. For the purpose of the study, an infected bedsore wound was defined as follows: (1) When there is a foul odor with dirty debris. (2) When bacterial swab or tissue culture results were “moderate” or “many,” along with identification of the bacteria strain. (3) Pseudomonas infection was clinically suspected when there was greenish discharge. Paralytic patients were excluded from this study. No patients received albumin or packed red blood cells (PRBC) transfusion during surgical debridement or flap surgery. Hemoglobin levels were raised to 10.0 g/dL by the day before the surgery.
We reviewed the medical records to determine the age, sex, comorbidities, pressure sore NPUAP staging, flap location, and flap size of each patient. These were compared across the groups. Preoperative and postoperative serum hemoglobin, neutrophil percentage, albumin, sodium, potassium, and Creactive protein (CRP) levels were recorded for each group, and changes over time were compared between groups. Changes in the number of albumin infusions and PRBC transfusions received each week from pre-operation to post-operation were also determined in each group. The preoperative values were obtained 1–7 days before surgery, and the postoperative values were obtained at 14 days after surgery. For patients who had repeated debridement, the results of the last blood test performed during hospitalization was considered as postoperative values.
ResultsThe study included a total of 63 patients: 53 in the flap coverage group and 10 in the control group. Age, sex, comorbidities, pressure sore grade, and size of flap were similar between groups (P>0.05, Mann-Whitney U test). The median (range) age was 74.2 years (range, 65–86 years) in the flap coverage group and 75.0 years (range, 65–94) years in the control group. The most common comorbidity in both groups was hypertension (n=30, 47.6%), followed by diabetes mellitus (n=29, 42.0%) and dementia, i.e., Parkinson’s disease (n=9, 14.3%) (Table 1). In the flap coverage group, 53 patients received a local myocutaneous flap and five patients received a local fasciocutaneous flap. The most common site of pressure sores was the sacrum, the second most common site was the greater trochanter of the femur, and the third most common site was the ischium. Across the two groups, five patients had multiple pressure ulcers on their bodies.
In the control group, there were no statistically significant changes in laboratory values before and after debridement (P>0.05, Wilcoxon signed-rank test). In the flap coverage group, the neutrophil percentage and CRP level improved significantly pre-operation to post-operation (P<0.05, paired ttest) (Table 2, Figs. 1, 2). The serum levels of hemoglobin, albumin and electrolytes did not differ with statistical significance from pre-operation to post-operation in either group (P>0.05, Wilcoxon signed-rank test and paired t-test). The number of albumin infusions and PRBC transfusions did not differ statistically significantly from preoperatively to postoperatively in either group (P>0.05, paired t-test).
DiscussionSacral pressure ulcers are the most common type of pressure sore and are caused by prolonged supine positioning, usually secondary to a general debilitated state. They typically occur in older people with major comorbidities. Because of the poor general health of these individuals, definitive surgical treatment is often avoided [2].
Appropriate management of grade III and IV pressure sores involves treating the underlying disease to prevent recurrence, optimizing the patient’s condition preoperatively, and performing a musculocutaneous flap or fasciocutaneous flap to cover the sore and add padding to the soft tissues in the area. If osteomyelitis is suspected, infected bone fragments should be removed, and reconstruction should be performed using a musculocutaneous flap with good blood flow.
The Physiological and Operative Severity Score for the enumeration of Morbidity and mortality (POSSUM) has been proposed as a method for standardizing patient data to allow direct comparison of patient outcomes, regardless of differing referral patterns and populations [5]. Copeland et al. [5] reported that the risk of surgery could be estimated by considering various physiologic and operative factors: age, cardiac history, respiratory history, blood pressure, pulse rate, Glasgow coma score, hemoglobin, white blood cell count, blood urea nitrogen, serum sodium and potassium, electrocardiogram results, operative severity, number of procedures (single vs. multiple), total blood loss, peritoneal soiling, presence of malignancy, and mode of surgery [6]. In a study of gluteus maximus fasciocutaneous flaps for sacral pressure sores in patients over 70 years of age, Mizumoto and Morita [7] found statistically significant differences in physiologic scores between patients with or without complications, but no differences in operative severity. Therefore, age as well as cardiovascular, respiratory, infection, electrolyte, and neurological status, should be considered before surgery in this patient population.
Before considering surgery in older patients with pressure sores, we ensure that concurrent diseases are optimized as much as possible to achieve and maintain normal vital signs. We provide nutritional support and administer electrolyte supplements, albumin infusions, and blood transfusions so that patients are in the best possible condition, despite the presence of existing diseases. Furthermore, in our clinical experience, the duration of the surgery is a very important determinant of postoperative complications when operating under general endotracheal anesthesia. Large amounts of anesthetic agents increase the possibility of postoperative atelectasis, lead to difficulties in maintaining ideal postoperative positioning, and reduce postoperative flap stability. Therefore, we limit the duration of operation for flap surgery in patients 70 years or older to 3 hours or less.
In the current study, in which we resected infected bone fragments to control infection and achieved stable coverage of osteomyelitis using muscle flaps, levels of hemoglobin, albumin, sodium, and potassium were not significantly different before and after surgery. This supports the practice of correcting medically-correctable factors of POSSUM to reduce surgical complications.
In 2010, Keys et al. [8] found that albumin levels below 3.5 g/dL were associated with ulcer recurrence within 1 year, suggesting that malnutrition should be corrected with high-protein diets and peripheral amino acid infusions, and nutritional markers, including albumin and prealbumin, should be monitored as a means of directing treatment [2]. In another study, the caloric deficit per day was higher in patients with successful pressure ulcer closure, although this finding did not achieve statistical significance [9].
Tangentially-split gluteus maximus myocutaneous flaps can be used to cover sacral sores while reducing functional loss. To further preserve the gluteal muscle, superior and inferior gluteal artery perforator flaps have also been successfully used for sacral, trochanteric, and ischial reconstruction [10]. Traditionally, musculocutaneous flaps have been preferred for their ability to (1) fill dead spaces, (2) provide an additional blood supply, and (3) add padding to soft tissue areas. However, since the introduction of perforator flaps, no difference in recurrence has been found between fasciocutaneous flaps and muscle flaps when used to treat pressure sores [11].
Despite the long history of research on pressure ulcer wound infections, the literature has focused on surgical techniques, with very few reports of pressure sore infections caused by antibiotic-resistant bacteria [12]. The traditional recommendation of 6–12 weeks of antibiotic therapy for chronic osteomyelitis, of which at least the first 2–6 weeks are intravenous, is increasingly challenged in favor of oral antibiotic treatment [13]. When osteomyelitis occurs with sacral pressure sores, the affected bone must be excised, and the vertebral sac must be preserved. The posterior superior iliac spine (PSIS) is a reliable landmark for localizing the S2–S3 junction and termination of the dural sac. Whenever possible, sacral debridement medial to the sacral foramina above the level of PSIS must be performed conservatively, avoiding aggressive debridement [14].
When osteomyelitis is more widespread, muscle flaps with an abundant blood supply can be expected to aid the killing of bacteria by neutrophils or macrophages [3]. In South Korea, rates of carbapenem-resistant Acinetobacter baumannii were 89.8% in 2013, and isolation rates for methicillin-resistant Staphylococcus aureus and vancomycin-resistant enterococci were 72% and 30%, respectively, in 2015 [15]. Most older patients with pressure sores are referred for surgery with grade IV ulcers, and the wounds have been open for a prolonged time, allowing them to become contaminated with multiple antibiotic-resistant bacteria.
With large, infected pressure sores, the neutrophil count is expected to be high, although in some cases, bone marrow depression occurs, producing a falsely normal neutrophil count. To avoid being misled by such a case, CRP and procalcitonin levels were also determined. Even if a normal neutrophil count leads to misinterpretation of the situation as being a nonsurgical condition, until the need for surgery is determined, patients should be prepared for the operation including a high-protein diet, administering PRBCs or albumin as appropriate, correcting electrolyte imbalances, and obtaining tissue (instead of swab) cultures.
For patients not expected to be able to walk within 3 days after the first debridement, we performed wide excision and a flap. Scarring around pressure sores is often severe, and if the wound edges coincide with this scar tissue, wound dehiscence is more likely to occur. Therefore, it is best to debride an area wide enough to allow for primary tissue repair. Also, considering the possibility that the body’s recovery process from other surgical procedures (including debridement) might overlap with the recovery of the flap, further studies assessing the effect of flap surgery on non-inflammatory markers, and clinical outcomes over a longer follow-up, will be needed in the future. In addition, a future study should include a control group at least as large as the flap coverage group.
In conclusion, older patients with multiple comorbidities and severe pressure sores who underwent surgery using myocutaneous or fasciocutaneous flaps recovered with better control of inflammatory markers. Laboratory findings consistent with infection decreased only in patients treated with a flap. Therefore, in patients for whom the risks of general anesthesia are not considered excessive, total debridement of pressure sores followed by myocutaneous or fasciocutaneous flap surgery is recommended instead of simple wound dressings or debridement.
Fig. 1.Debridement and bilateral gluteus maximus myocutaneous flaps. A 70-year-old female was bedridden for 6 months because of severe dementia. She underwent pressure sore surgery in the sacral area with a bilateral gluteus maximus myocutaneous flap. The flap size was approximately 14×12 cm. The photographs were obtained preoperatively (A), intraoperatively (B), immediately after surgery (C), and 2 weeks after surgery (D). 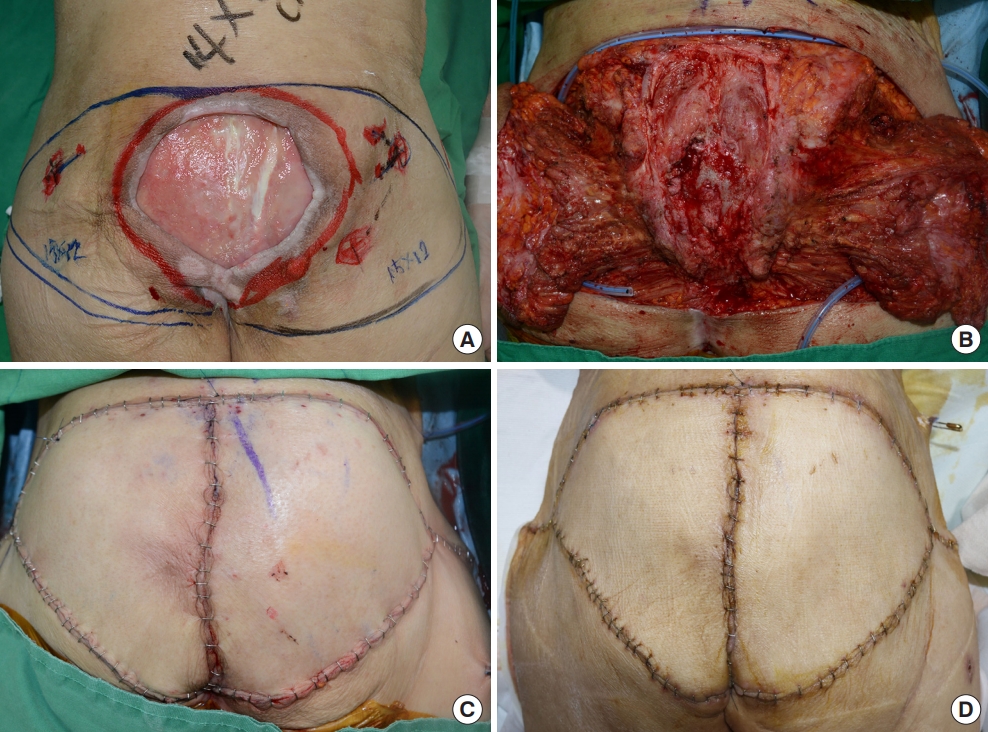
Fig. 2.Debridement and bilateral gluteus maximus myocutaneous flaps and posterior thigh fasciocutaneous flaps. A 65-year-old female with a previous cerebrovascular accident, hypertension, diabetes mellitus, chronic kidney disease, and heart failure was referred to our department for surgery. Stage IV pressure sores on the sacrum (12×12 cm) and left ischium (2×2 cm) were covered with a bilateral gluteus maximus myocutaneous flap and posterior thigh fasciocutaneous flap, respectively. The photographs were obtained preoperatively (A, B), immediately after surgery (C), and 2 weeks after surgery (D). 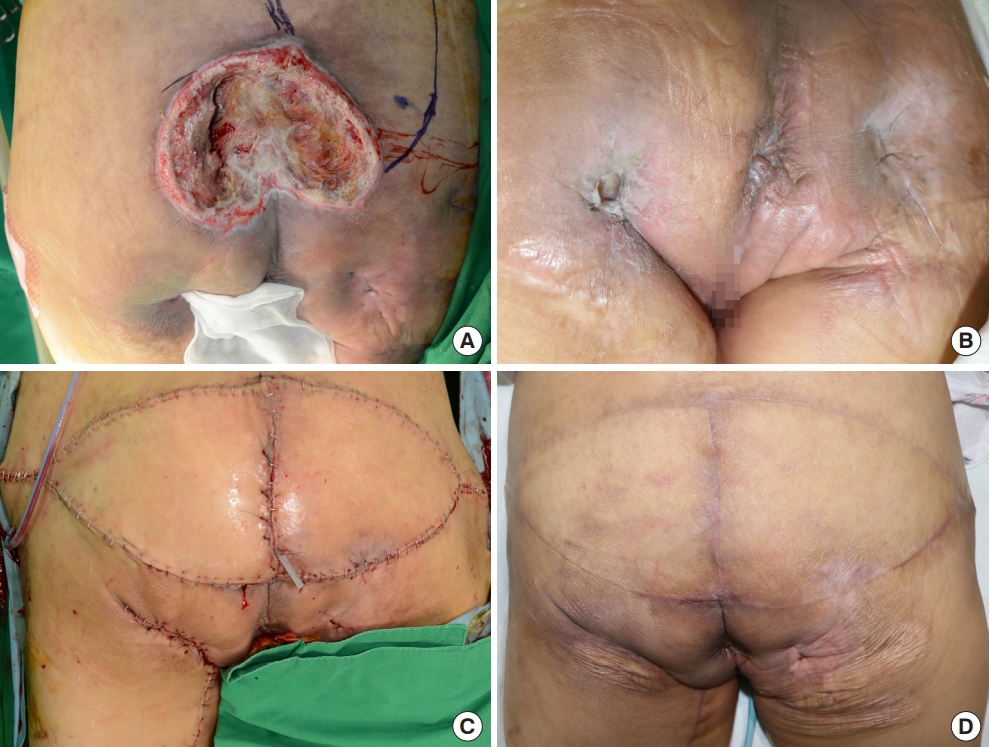
Table 1.Patient characteristics Table 2.Before and after general wound care (debridement only) and flap surgery (debridement and flap surgery) for pressure ulcers References1. Jaul E, Barron J, Rosenzweig JP, et al. An overview of comorbidities and the development of pressure ulcers among older adults. BMC Geriatr 2018;18:305.
2. Kwon R, Rendon J, Janis JE. Pressure sores. In: Song DH, Neligan PC, editors. Plastic surgery. 4 ed. New York: Elsevier; 2018. p. 350-79.
3. Mathes SJ, Alpert BS, Chang N. Use of the muscle flap in chronic osteomyelitis: experimental and clinical correlation. Plast Reconstr Surg 1982;69:815-29.
4. Friederichs J, Hutter M, Hierholzer C, et al. Procalcitonin ratio as a predictor of successful surgical treatment of severe necrotizing soft tissue infections. Am J Surg 2013;206:368-73.
5. Copeland GP, Jones D, Walters M. POSSUM: a scoring system for surgical audit. Br J Surg 1991;78:355-60.
6. Whiteley MS, Prytherch DR, Higgins B, et al. An evaluation of the POSSUM surgical scoring system. Br J Surg 1996;83:812-5.
7. Mizumoto K, Morita E. Evaluation of the Physiological and Operative Severity Score for the Enumeration of Mortality and Morbidity (POSSUM) scoring system in elderly patients with pressure sores undergoing fasciocutaneous flap-reconstruction. J Dermatol 2009;36:30-4.
8. Keys KA, Daniali LN, Warner KJ, et al. Multivariate predictors of failure after flap coverage of pressure ulcers. Plast Reconstr Surg 2010;125:1725-34.
9. Auiwattanakul S, Ungpinitpong W, Yutthakasemsunt S, et al. Prevalence of pressure ulcer and nutritional factors affecting wound closure success in Thailand. Mater Sociomed 2017;29:196-200.
10. Levine SM, Sinno S, Levine JP, et al. Current thoughts for the prevention and treatment of pressure ulcers: using the evidence to determine fact or fiction. Ann Surg 2013;257:603-8.
11. Thiessen FE, Andrades P, Blondeel PN, et al. Flap surgery for pressure sores: should the underlying muscle be transferred or not? J Plast Reconstr Aesthet Surg 2011;64:84-90.
12. Jugun K, Richard JC, Lipsky BA, et al. Factors associated with treatment failure of infected pressure sores. Ann Surg 2016;264:399-403.
13. Spellberg B, Lipsky BA. Systemic antibiotic therapy for chronic osteomyelitis in adults. Clin Infect Dis 2012;54:393-407.
|
|